I have just been reading about this in relation to PWD when in hospital for unrelated conditions, just wondered if anyone else heard about it, and opinions??
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
JOHN'S CAMPAIGN
- Thread starter maryjoan
- Start date
I had not heard of it, Google has-
https://johnscampaign.org.uk/#/
You can check whether a trust or individual hospital has signed up, whether signing up and practising are the same maybe a different matter.
All My trust has
https://johnscampaign.org.uk/#/
You can check whether a trust or individual hospital has signed up, whether signing up and practising are the same maybe a different matter.
All My trust has
Last edited:
I've been talking about this for years. It's been set up by the famous writer Nikki Gerrard. John was her father, and she had a terrible time with visiting hours when he was very ill in hospital. I think it's a very good thing she is doing and a lot of hospitals have signed up for it now, though sometimes it doesn't get communicated down to the coalface enough, to snippy ward sisters who think they can still tell people when to visit, even though as a carer you should have open visiting times. You wouldn't say this in a children's ward so why say it with the vulnerable and elderly?
Her books are really good too, btw! She writes a lot as Nicci French, together with her husband, Sean French.
Her books are really good too, btw! She writes a lot as Nicci French, together with her husband, Sean French.
Last edited:
I had not heard of it, Google has-
https://johnscampaign.org.uk/#/
You can check whether a trust or individual hospital has signed up, whether signing up and practising are the same maybe a different matter.
All My trust has
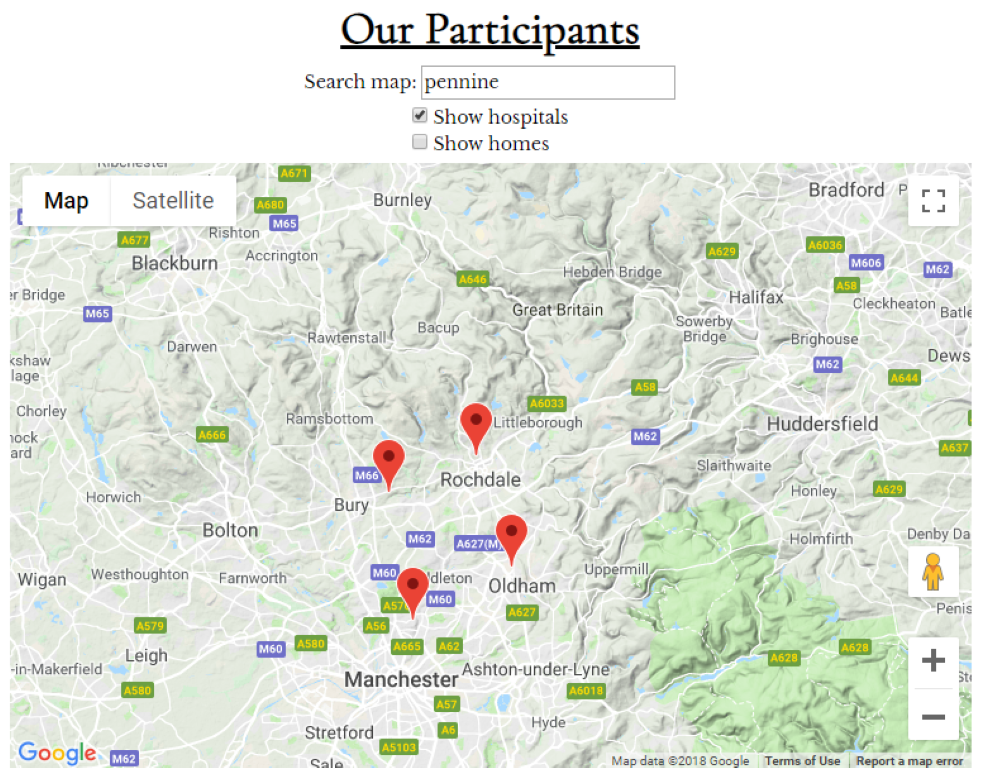
View attachment 60064
Aye up! You've got my home town on there - Farnworth - went to school in Bury. Perhaps I should move back north??
I'm S bury, went to school in Derby
Since you change your location a few weeks ago you appear to now live in
https://forum.alzheimers.org.uk/misc/location-info?location=South+of+the+Border
Since you change your location a few weeks ago you appear to now live in
https://forum.alzheimers.org.uk/misc/location-info?location=South+of+the+Border
Last edited:
Aye, I changed location because of privacy thoughts after being on BBC TV Breakfast.I'm S bury, went to school in Derby
Since you change your location a few weeks ago you appear to now live in
https://forum.alzheimers.org.uk/misc/location-info?location=South+of+the+Border
There was a thread about it on TP in 2015.
https://forum.alzheimers.org.uk/threads/johns-campaign.78670/
https://forum.alzheimers.org.uk/threads/johns-campaign.78670/
I was not aware of this campaign, but last time C was in hospital the visiting hours had been extended to allow visitors pretty much any time from 11 until 9 at night with polite requests not to tire out the patient. It gave me more hope of being there at mealtimes if needed, though thankfully she was out before it was tested. Still, after the hassle of previous stays it was a move in the right direction.
Aaaggggghhhhhh! I am so exhausted and fed up, and my sister is currently in tears as we are unable to get to speak to doctors for my dad, who has dementia and is currently in hospital. He has a fractured spine which can't be fixed and is experiencing waves of pain every four mins or so which leave him purple, gurning and crying with pain for about 45 seconds at a time. The multidisciplinary team conclude he's 'medically fit'. How can someone be medically fit when they are in so much pain that if he was in his care home they would be dialling 999? All the staff at the hospital are individually sympathetic and understanding, but it is the SYSTEM which is driving us nuts. It is completely un joined up. So much for all these billions spent on IT systems in hospital. No information ever seems to be available.
Our biggest problem, hence the addition to this thread, is that visiting times are 1-3pm and 5-7pm. Dad is too tired and sleepy by 5pm, so no point sitting by his bedside really then as he just gets cross and wants us to go. Doctors' rounds are at 9.30am ish, but it is insane that no nurses accompany the docs to explain what dad is going through. When the doc asks dad how he is, he answers 'I think I'm all right, aren't I?' because as soon as the wave of pain has gone, he has forgotten about it. Fortunately on Weds night the dementia nurse happened to be on the ward when the doc was there, witnessed that dad had said he was ok, and asked the doc to wait until dad was having a pain spasm. If she hadn't done that, the docs would have no idea that dad even HAD any pain. I can't believe in 2018 with all the understanding of dementia etc these days that we are not allowed to be on the ward at doc round time to advocate for our father. We have POA so we are legally HIM in this respect and surely have a right to be there so long as we don't get in the way? All the hospital keep saying is phone to make an appointment with the doctor, but this is proving extremely difficult with no answers from sec office etc. The refuse to give us the SHO name who saw him, just give us the Consultant name but won't give us a phone number or email for her, just keep saying phone her secretary. I spoke to the discharge lady this morning, who is aware of dad's issues and is present at the daily multidisciplinary meeting, and she says he won't be discharged till the pain is under control, but we keep getting conflicting info on the ward, who are requesting that we get dad's care home in to assess him now. If the care home people come now they will refuse to take him as they can't cope with this level of pain (they have said this). We are also awaiting the results of a bone scan taken 1 WEEK AGO TODAY (!) to see if he has prostate cancer and possibly metastases on his spine causing more pain.
Is it me??!!! I wonder how many thousands of dementia patients are in hospital with no-one speaking for them due to these stupid rules preventing relatives attending doc's visits.
How can this be?
Frustrated beyond belief and very worried about my dad.
Our biggest problem, hence the addition to this thread, is that visiting times are 1-3pm and 5-7pm. Dad is too tired and sleepy by 5pm, so no point sitting by his bedside really then as he just gets cross and wants us to go. Doctors' rounds are at 9.30am ish, but it is insane that no nurses accompany the docs to explain what dad is going through. When the doc asks dad how he is, he answers 'I think I'm all right, aren't I?' because as soon as the wave of pain has gone, he has forgotten about it. Fortunately on Weds night the dementia nurse happened to be on the ward when the doc was there, witnessed that dad had said he was ok, and asked the doc to wait until dad was having a pain spasm. If she hadn't done that, the docs would have no idea that dad even HAD any pain. I can't believe in 2018 with all the understanding of dementia etc these days that we are not allowed to be on the ward at doc round time to advocate for our father. We have POA so we are legally HIM in this respect and surely have a right to be there so long as we don't get in the way? All the hospital keep saying is phone to make an appointment with the doctor, but this is proving extremely difficult with no answers from sec office etc. The refuse to give us the SHO name who saw him, just give us the Consultant name but won't give us a phone number or email for her, just keep saying phone her secretary. I spoke to the discharge lady this morning, who is aware of dad's issues and is present at the daily multidisciplinary meeting, and she says he won't be discharged till the pain is under control, but we keep getting conflicting info on the ward, who are requesting that we get dad's care home in to assess him now. If the care home people come now they will refuse to take him as they can't cope with this level of pain (they have said this). We are also awaiting the results of a bone scan taken 1 WEEK AGO TODAY (!) to see if he has prostate cancer and possibly metastases on his spine causing more pain.
Is it me??!!! I wonder how many thousands of dementia patients are in hospital with no-one speaking for them due to these stupid rules preventing relatives attending doc's visits.
How can this be?
Frustrated beyond belief and very worried about my dad.
I really sympathise with your problems. To cut a long story short, Mum also had a fractured spine but the hospital failed to identify this. They stated that her sudden inability to stand/walk was due to 'dementia'. She was in a great deal of pain. The doctors initially stated that this was due to 'spending too long in bed', then denied that she was in pain, recording 'daughter thinks she can gauge Mum's pain better than anyone but we have pain chart' Yes, but it wasn't being filled in properly and staff didn't know Mum!!! Mum subsequently spent 3 months in hospital, having walked into A&E for treatment to a cut eyebrow. They still hadn't identified the cause of her pain by the time she was discharged. When I took the afternoon off work to speak to a consultant I was left waiting for 3 hours then informed that he had gone home. I eventually spoke to the doctors by turning up first thing in the morning and waiting for them to arrive, so they couldn't avoid me. I also have H&W POA. There is a lengthy complaint going to the hospital and Quality Care Commission......
Go to the PALS team at the hospital, explain what's going on and demand that you are allowed to visit your Dad outside of normal visiting hours. My complaint to PALS got passed up to a director as the ward wouldn't respond to PALS and that got things moving for a while. It's awful that families have to resort to this just to get adequate care for patients with dementia but don't give up. Keep on at them!
Go to the PALS team at the hospital, explain what's going on and demand that you are allowed to visit your Dad outside of normal visiting hours. My complaint to PALS got passed up to a director as the ward wouldn't respond to PALS and that got things moving for a while. It's awful that families have to resort to this just to get adequate care for patients with dementia but don't give up. Keep on at them!
Hi , Sadly my mam passed away nearly a year ago . My sister and I took it in turns to stay with mam when she was in hospital with aspiration pneumonia. Not one person questioned us all the nurses were really helpful. My sister was given a pull out bed in one ward on another ward it was just a chair but they offered extra blankets and the use of tea making facilities. We would never have left mam because she could not communicate we were her voice . Reguarding pain that Alzheimer patients suffer I still think the medical profession have a long way to go at addressing this .
Our late mum was reasonably OK in hospital, where staff were more aware of dementia etc, but problems started when she was moved to a 'community ward' in a different hospital, for patients who were medically fit but unable to leave for other reasons, and run by a private company. I think the 'medically fit' label led staff to believe that they had no other problems either. There were hardly any clinical staff and the patients were mostly just left to their own devices with very little monitoring - not great for PWDs and the elderly, which accounted for most of them. It's sad that although there's more general awareness of dementia there still seems to be a lack of practical measures to make life easier for PWDs in hospital.
On the verge of doing that. Waiting to see if we can see doc. To be fair, we did get an appointment one week ago, but this morning even the sec isn't calling us back. Obvs it's going to be weekend now, but if we don't get any further, I will just take up position on a chair brought from home (camping stool - always goes to hospital with me!) outside the ward door on Monday morning, and will tag along with the doc, kicking and screaming if necessary, so I can be there when they examine dad.I really sympathise with your problems. To cut a long story short, Mum also had a fractured spine but the hospital failed to identify this. They stated that her sudden inability to stand/walk was due to 'dementia'. She was in a great deal of pain. The doctors initially stated that this was due to 'spending too long in bed', then denied that she was in pain, recording 'daughter thinks she can gauge Mum's pain better than anyone but we have pain chart' Yes, but it wasn't being filled in properly and staff didn't know Mum!!! Mum subsequently spent 3 months in hospital, having walked into A&E for treatment to a cut eyebrow. They still hadn't identified the cause of her pain by the time she was discharged. When I took the afternoon off work to speak to a consultant I was left waiting for 3 hours then informed that he had gone home. I eventually spoke to the doctors by turning up first thing in the morning and waiting for them to arrive, so they couldn't avoid me. I also have H&W POA. There is a lengthy complaint going to the hospital and Quality Care Commission......
Go to the PALS team at the hospital, explain what's going on and demand that you are allowed to visit your Dad outside of normal visiting hours. My complaint to PALS got passed up to a director as the ward wouldn't respond to PALS and that got things moving for a while. It's awful that families have to resort to this just to get adequate care for patients with dementia but don't give up. Keep on at them!
What a crock.
How did they manage your mum's pain in the end? Isn't is insane that they ask someone with dementia to describe their pain - when dad isn't in pain, he forgets instantly that it's been there (good and bad - I'm glad he's not lying there terrified about the advent of the next horrendous spasm, but it means he thinks he's fine in the intervening minutes, which always seems to be when the doc is there or a nurse asks him if he feels any pain). Dad has started a couple of days ago on morphine patches (dementia nurse said she had to fight personally for this due to the high cost - bless her). He can't go back to care home with oromorph apparently, but this hasn't been working anyway. Patches are known to take several days to kick in, and hadn't up to last night when I left him. Codeine helped but makes him constipated, even with laxative and lactulose, and he is in way too much pain to push a hard poo out. Dementia nurse also worried that all painkillers available except paracetamol have adverse affects on dementia and confusion levels. I said to her I'm less worried about confusion (which is ever present anyway - poor old soul has no idea where he is at any time anyway) and more about pain, which is unbearable for dad and horrendous for anyone who cares about him to witness (which currently only appear to be me, my sis and the dementia nurse - everybody else seems to ignore him crying out in pain every four or five mins, except the night staff who helpfully left THREE handwritten notes on his nightstand asking him to be quiet because he was disturbing the other patients. Seriously).
I'm about to get in the car and trundle the 1.5 hrs up the road for today's fun and games. I'll check in here again later.
My sister has written to PALS. No response as yet. We never got a callback from the Consultant's sec. How bad it that? We eventually met with the SHO who confirmed that dad will NOT be discharged (no-one has taken responsibility for cancelling the care home visit to assess though, so we've done that). She also said we can call the Consultant's sec and ask for an appointment to discuss dad at any time. We told her there is an answerphone and no callback and she looked puzzled. Not sure what else to do about this except loiter around by the ward door and pounce on doctor unannounced, which doesn't seem right or sensible. Anyway, it's the weekend now so nothing will happen for next 2 days. Dad still writhing around in pain as at 5pm yesterday. He didn't want us to go, but in the end we just had to walk away while he cried and shouted at us. God, I hate all this.I really sympathise with your problems. To cut a long story short, Mum also had a fractured spine but the hospital failed to identify this. They stated that her sudden inability to stand/walk was due to 'dementia'. She was in a great deal of pain. The doctors initially stated that this was due to 'spending too long in bed', then denied that she was in pain, recording 'daughter thinks she can gauge Mum's pain better than anyone but we have pain chart' Yes, but it wasn't being filled in properly and staff didn't know Mum!!! Mum subsequently spent 3 months in hospital, having walked into A&E for treatment to a cut eyebrow. They still hadn't identified the cause of her pain by the time she was discharged. When I took the afternoon off work to speak to a consultant I was left waiting for 3 hours then informed that he had gone home. I eventually spoke to the doctors by turning up first thing in the morning and waiting for them to arrive, so they couldn't avoid me. I also have H&W POA. There is a lengthy complaint going to the hospital and Quality Care Commission......
Go to the PALS team at the hospital, explain what's going on and demand that you are allowed to visit your Dad outside of normal visiting hours. My complaint to PALS got passed up to a director as the ward wouldn't respond to PALS and that got things moving for a while. It's awful that families have to resort to this just to get adequate care for patients with dementia but don't give up. Keep on at them!
Reading posts this morning I am feeling outraged whether it is filling in a document with volume of pee and description of poo to your father being given hand written notes to keep quiet.
It is as if these people never read or think about anything to do with dementia even though it is the biggest medical issue of our age.
I find that the best care workers John has in his day care are the ones who have or had parents with dementia. I don’t need to spell out the problems to them. They get it immediately and all agree that when the problem is in your own family you see the whole picture forcefully.
It is as if these people never read or think about anything to do with dementia even though it is the biggest medical issue of our age.
I find that the best care workers John has in his day care are the ones who have or had parents with dementia. I don’t need to spell out the problems to them. They get it immediately and all agree that when the problem is in your own family you see the whole picture forcefully.
There is supposed to be a Multidisciplinary Team Meeting to discuss patients. This meeting, as the name suggests, should include representatives from surgical teams, nursing teams, in fact all the various teams that are involved in a patient's care. Ask the Ward Manager (or whatever they call them in your Trust) for a copy of the MDT notes that include your father. Whether you have POA or not, if you are next of kin they should respond to this. They may not have to disclose them to you (not sure if this is something they can freely share with you as my experience is only when solicitors get involved and they are asked to disclose these meeting notes) but it will alert them to the fact that they should be discussing your father at these meetings. Nurses will know that your father is suffering pain in these waves and should be reporting it to the meeting, at which the doctors/consultant should be present.
How did they manage your mum's pain in the end?
I had to keep pushing for effective pain relief but it wasn't easy. When I pointed out that Mum was clearly in severe pain when sitting in the chair they prescribed pain relief 'only when sitting in chair'!! They then carried on assessing for pain when Mum was in bed (when the pain was reduced). Mum was on Codeine and they eventually doubled the dose. After 7 weeks of not being able to stand up/walk Mum then got up and walked. The doctors stated that this was due to 'fluctuating dementia' and they hadn't increased the pain relief earlier as it might have negatively affected her mobility.... They then put her on a morphine patch which resulted in her being over-sedated (comatose), unable to mobilise or eat/drink. They refused to reduce/stop the morphine due to 'pain', despite previously insisting that she was not in any pain. They kept asking how I knew Mum was in pain, as if I was making it up. Er, the tears in her eyes, wincing, screaming, reaching to touch her back, looking like she was in pain, sudden inability to stand up/walk and saying that her back hurt were a bit of a give away. The dementia nurse and physio also reported that Mum was in pain but the medical team still didn't seem to believe this. The refused to carry out an x-ray on the grounds 'it would be too hard on her back'.
Mum is now back on the codeine and the constipation is being managed with a daily laxative. Out of the various pain relief meds tried the codeine worked the best in terms of effective pain relief and least side-effects but it can be a case of 'trial & error' to identify which works best. Mum became homeless during her hospital stay as her residential home asked for an assessment and the hospital didn't do one. The doctor stated 'we wouldn't have this problem if you looked after Mum yourself'. She has now had to move to a nursing home. Hopefully things won't get that bad for your Dad but I agree that it is awful to see someone in pain whilst those that should be caring stand by and do very little. I wish you luck with the battles ahead.
Thanks. We battle on.I had to keep pushing for effective pain relief but it wasn't easy. When I pointed out that Mum was clearly in severe pain when sitting in the chair they prescribed pain relief 'only when sitting in chair'!! They then carried on assessing for pain when Mum was in bed (when the pain was reduced). Mum was on Codeine and they eventually doubled the dose. After 7 weeks of not being able to stand up/walk Mum then got up and walked. The doctors stated that this was due to 'fluctuating dementia' and they hadn't increased the pain relief earlier as it might have negatively affected her mobility.... They then put her on a morphine patch which resulted in her being over-sedated (comatose), unable to mobilise or eat/drink. They refused to reduce/stop the morphine due to 'pain', despite previously insisting that she was not in any pain. They kept asking how I knew Mum was in pain, as if I was making it up. Er, the tears in her eyes, wincing, screaming, reaching to touch her back, looking like she was in pain, sudden inability to stand up/walk and saying that her back hurt were a bit of a give away. The dementia nurse and physio also reported that Mum was in pain but the medical team still didn't seem to believe this. The refused to carry out an x-ray on the grounds 'it would be too hard on her back'.
Mum is now back on the codeine and the constipation is being managed with a daily laxative. Out of the various pain relief meds tried the codeine worked the best in terms of effective pain relief and least side-effects but it can be a case of 'trial & error' to identify which works best. Mum became homeless during her hospital stay as her residential home asked for an assessment and the hospital didn't do one. The doctor stated 'we wouldn't have this problem if you looked after Mum yourself'. She has now had to move to a nursing home. Hopefully things won't get that bad for your Dad but I agree that it is awful to see someone in pain whilst those that should be caring stand by and do very little. I wish you luck with the battles ahead.
Yes there is a daily meeting, and it now seems that all included in that meeting now agree dad's pain is bad, needs to be sorted and that he shouldn't be discharged until that has happened. But we still get comments from the nurses and discharge team that he is medically fit. Discharge lady now says definitely no discharge till pain under control, but certain members of staff don't seem to have got the message and so we are getting occasional conflicting communication which naturally makes us worried. We are now, however, reassured by the SHO that he will not be discharged until pain is hopefully less and can be managed by care home staff, but so far he has had the morphine patch since Tues and it was increased from 5mg to 10mg on Weds, but as at last night he was still having these horrendous contraction-type spasms of pain which make him cry for help for about 40 secs ever 4-5 mins. The nursing staff must have hearts of steel because they completely ignore his cries for help but, since there's nothing they can do for him, I suppose they would 'waste' a lot of time comforting him if he's getting all the help that is available at the moment and they have got enough to do. There are members of staff (healthcare assistants) stationed next to other patients 24/7 on dad's ward as they are in danger of hurting themselves if they try to get out of bed, and these members of staff just sit there and listen as dad cries out in pain. It's hard to watch, but I suppose they are only doing the job they are assigned to by the nurse and cannot interfere. As his daughter, I find it very distressing, and I would find it extremely unsettling if I were a patient on the ward or a visitor to the ward.There is supposed to be a Multidisciplinary Team Meeting to discuss patients. This meeting, as the name suggests, should include representatives from surgical teams, nursing teams, in fact all the various teams that are involved in a patient's care. Ask the Ward Manager (or whatever they call them in your Trust) for a copy of the MDT notes that include your father. Whether you have POA or not, if you are next of kin they should respond to this. They may not have to disclose them to you (not sure if this is something they can freely share with you as my experience is only when solicitors get involved and they are asked to disclose these meeting notes) but it will alert them to the fact that they should be discussing your father at these meetings. Nurses will know that your father is suffering pain in these waves and should be reporting it to the meeting, at which the doctors/consultant should be present.
I just find it weird that these members of staff who work day in day out with dementia patients are so unprepared for dealing with them. I know each dementia patient is different, but I am daily amazed by their lack of understanding and empathy. I am, of course, extremely sensitive to everything at the moment, being in such awful circumstances and watching my dad's confusion and pain, so I may be being overly critical, and when all this is over maybe I'll look back and think they were just doing the best they could in difficult circumstances. Only time will tell. At the moment I want to shout and scream.Reading posts this morning I am feeling outraged whether it is filling in a document with volume of pee and description of poo to your father being given hand written notes to keep quiet.
It is as if these people never read or think about anything to do with dementia even though it is the biggest medical issue of our age.
I find that the best care workers John has in his day care are the ones who have or had parents with dementia. I don’t need to spell out the problems to them. They get it immediately and all agree that when the problem is in your own family you see the whole picture forcefully.
I thought it was ironic that staff referred family to the dementia team 'so that they can understand dementia' when they clearly had little understanding themselves  . It was really worrying that every issue was put down to 'dementia'.
. It was really worrying that every issue was put down to 'dementia'.
Hopefully your Dad's pain will reduce with the patch. It usually takes 3 days for it to get to fuĺl strength.
Hopefully your Dad's pain will reduce with the patch. It usually takes 3 days for it to get to fuĺl strength.
